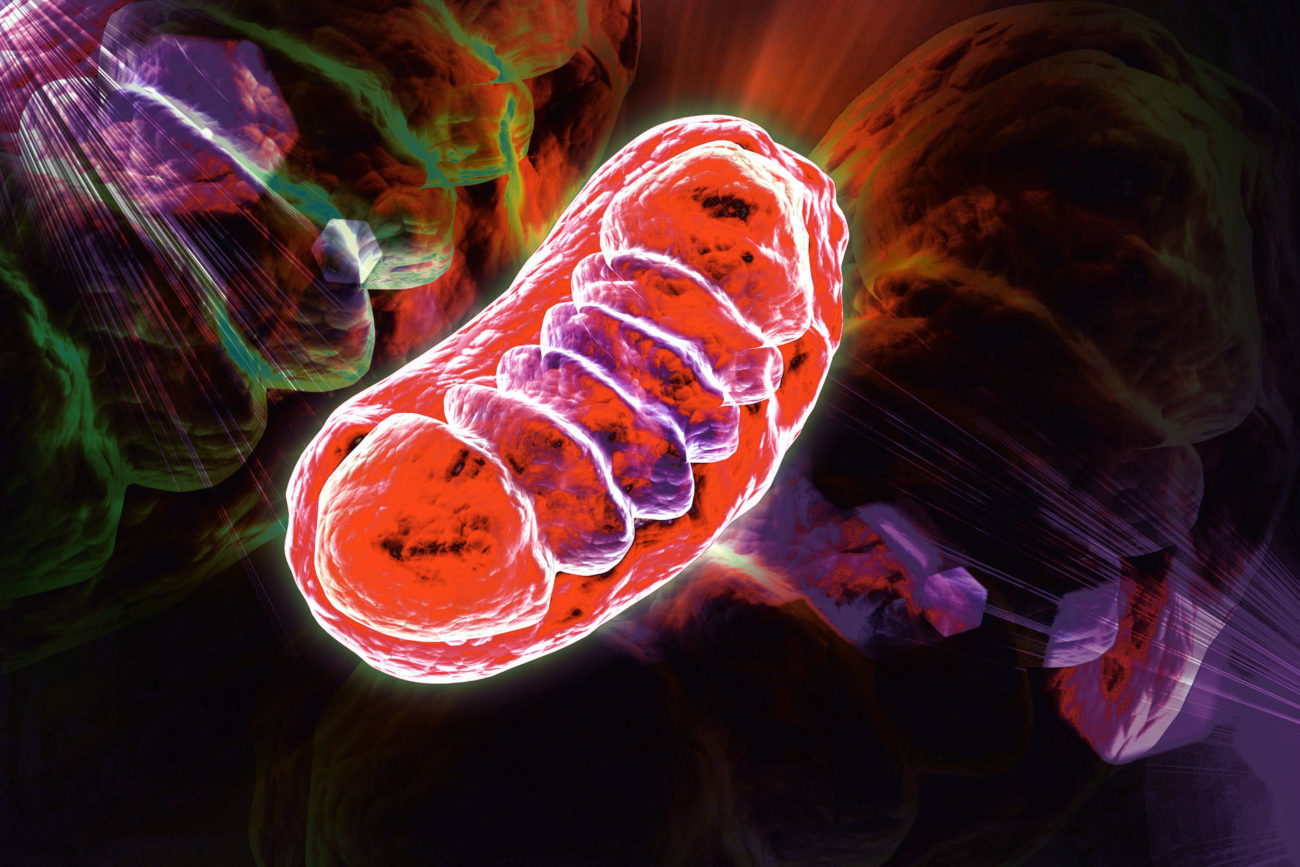
The mitochondria can be considered as the engine and energy source of cells. The mitochondria give us the amount of energy we need to move, grow and think. Mitochondria also play a crucial role in protecting the cells of the body against various types of damage.
Mitochondrial disease is serious and debilitating
Mitochondrial disease can occur when the mitochondria do not function properly. The disease is caused by congenital genetic variants and have a variable age of onset, although it often presents in early childhood. Sometimes, the symptoms arise from just one organ, but more often several organs or organ systems are involved, and the bodily functions worsen as the disease progresses. Typically affected organs are those with a high energy demand such as skeletal muscles, heart, brain, and endocrine organs. In the Voice of the patient Report 2019, patients with mitochondrial disease highlighted the large need for new effective treatments to improve bodily functions, stop disease progression and reduce debilitating symptoms with a high impact on daily living such as fatigue and muscle weakness.
What is mitochondrial disease?
Large need for mitochondrial treatments
There are no approved drug treatments for primary mitochondrial disease, except for a hereditary form of mitochondrial eye disorder, LHON (Leber’s Hereditary Optic Neuropathy), where Raxone® (idebenone) is approved in Europe and Israel. Despite this advancement, there is an enormous remaining unmet medical need.

“The fatigue is almost impossible to describe because it seems other-worldly. It feels as though someone has taped cinder blocks to my eyelids some mornings and there is no way to keep them open”.
From UMDF’s Voice of the patient Report, 2019
MELAS-MIDD and KSS-CPEO spectrum disorders
The MELAS (mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes) – MIDD (maternally inherited DNA depletion) spectrum disorder and KSS (Kearns-Sayre Syndrome) – CPEO (Chronic Progressive External Ophthalmoplegia Syndrome) spectrum disorder are mainly caused by the mitochondrial DNA (mtDNA) mutation m.3243A>G, or large deletions in the mtDNA.
Patients with these disorders often suffer from debilitating symptoms such as chronic fatigue, muscle weakness, deafness, and/or metabolic dysfunction.
MELAS-MIDD affects about 35 in 1,000,000 people. and KSS-CPEO affects about 15 in 1,000,000 people.
MERRF
MERRF (Myoclonic epilepsy with ragged-red fibers) is a primary mitochondrial disease with symptoms such as involuntary muscle twitching, difficulty coordinating muscle movements, and epilepsy but the disease can also affect many other functions. When examined under a microscope the muscle tissue has characteristic changes. The disease is caused by mutations in the mitochondrial DNA, mainly the mutation m.8344A>G.

“I am devastated just thinking about what his future might look like. No one wants to lose their child but also no one should have to suffer so much”.
From UMDF’s Voice of the patient Report, 2019
Leigh syndrome
Leigh Syndrome is a devastating inherited primary mitochondrial disease affecting children in their first years of life leading to severe progressive disability or childhood death. The disease onset typically occurs by the age of one to two years when first symptoms begin to develop, often during a period of illness or infection. After onset, the patients get worse in episodes and the disease typically leads to early death, with patients reaching a median age of 2.4 years.
Leigh Syndrome could be seen as a severe model of normal aging, primarily affecting the central nervous system, usually leading to loss of most of the functions of the brain and other main organs. Symptoms in other organ systems with high energy requirements are common.
In a majority of cases, Leigh Syndrome is caused by genetic mutations causing dysfunction of the mitochondrial respiratory complex I (CI) , which is critical for cell energy production. Defects in CI are the most common enzymatic defects also in mitochondrial diseases in general, accounting for 50% or more of the cases.
The estimated incidence of Leigh and Leigh-like Syndrome is 1:11,000 – 1:34,000 in every child born.
LHON
Leber’s Hereditary Optic Neuropathy (LHON) is a disease caused by mitochondrial DNA mutations in subunits of mitochondrial respiratory complex I (CI). This results in dysfunctional cell energy production, leading to degeneration of the retinal ganglion cells and loss of central vision. LHON most commonly affects males in their second or third decade of life. There are approximately 25,000 people with LHON in Europe.
Different Types of Mitochondrial Disease
Read more about the different types of primary mitochondrial disease, on the US patient organization UMDF’s website